What is Fungal Acne, and How do I Treat It?
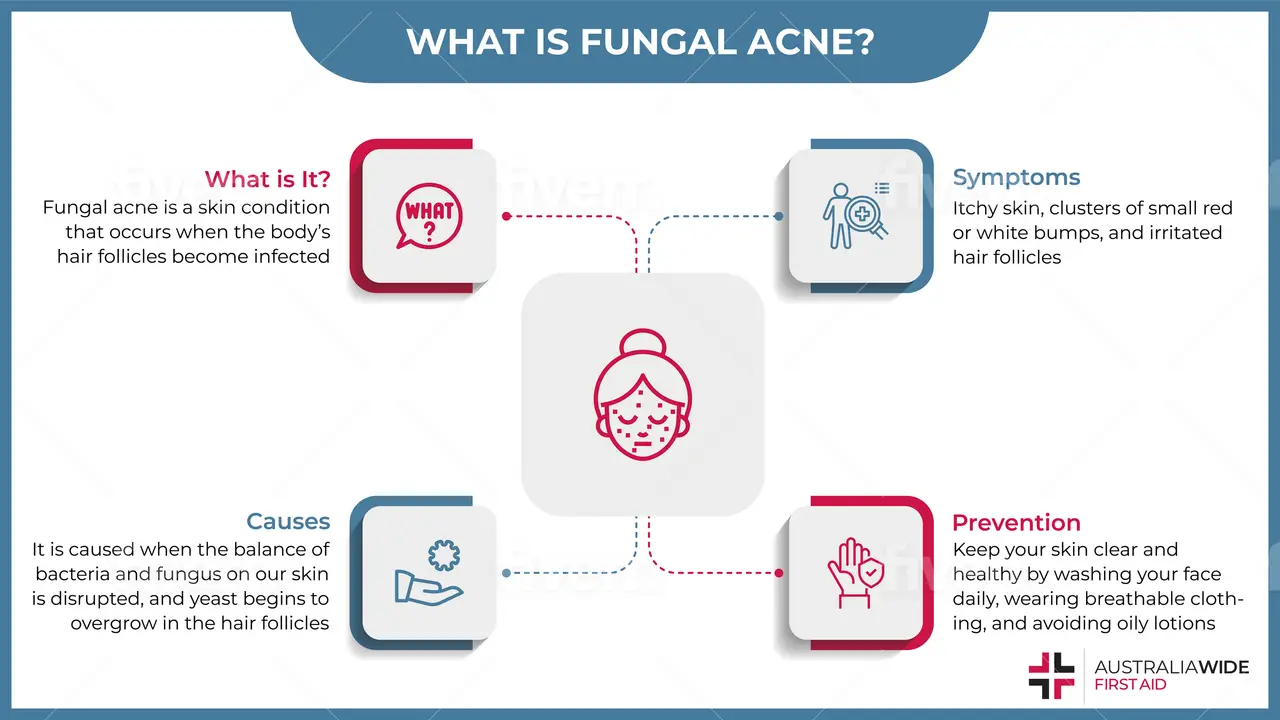
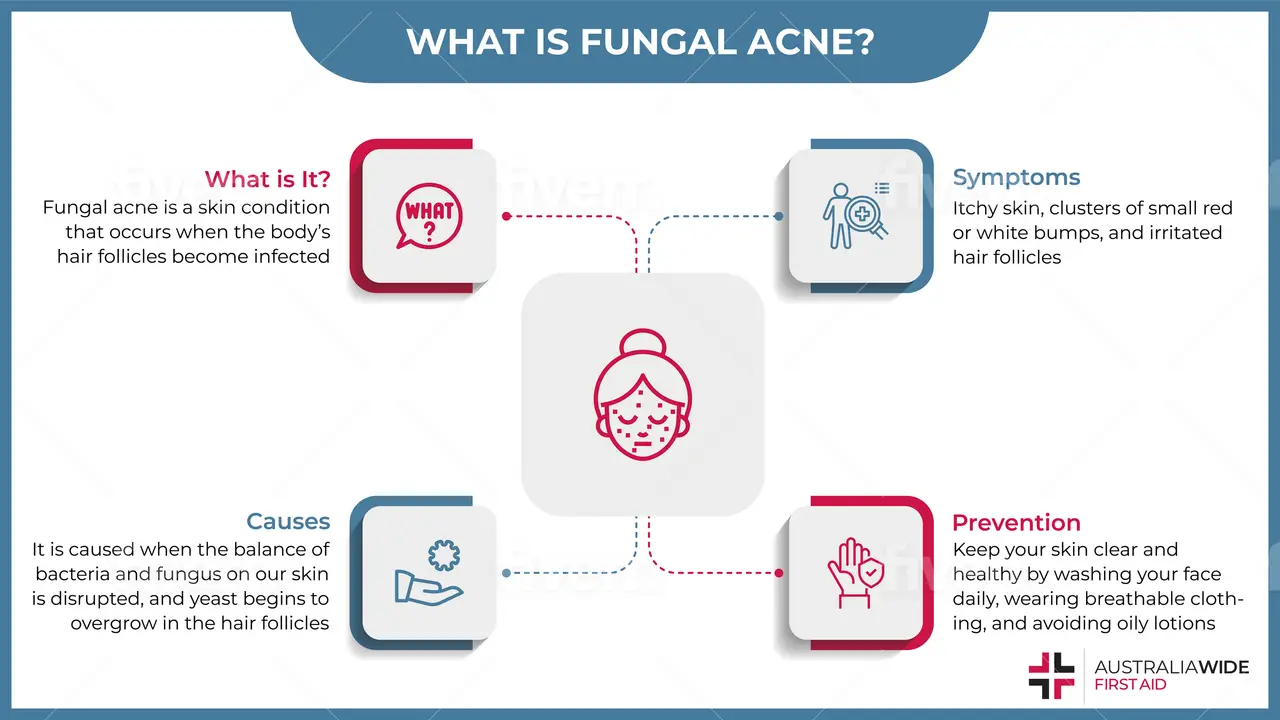
Contrary to popular belief, fungal acne is not acne – but rather a skin condition caused by an infection of the hair follicle.
Fungal acne can often look like pimples and is often confused with bacterial acne.
Fungal acne is a skin condition called pityrosporum folliculitis that causes an infection in the body’s hair follicles. Folliculitis causes the hair follicles to become inflamed and infected therefore causing small bumps filled with pus to appear on the skin. It can show up anywhere on the skin, except for the palms of your hands and soles of your feet.
Due to its similarities with facial acne, fungal acne is often mistaken as bacterial acne and doesn’t get better with treatment. This is usually a sign that a fungal infection may be present in the hair follicle.
Anyone can get fungal acne, however, it usually affects teenagers because of the extra oil production in the skin – feeding the yeast that causes fungal acne. It is often found on the shoulders, back, and neck and can be caused by sweating.
Fungal acne is mainly caused by an overgrowth of yeast in the hair follicles. The yeast responsible for fungal acne is always present on our skin and typically, our body and immune system does an excellent job in keeping them in check.
However, an overgrowth can occur if your immune system is unable to keep up with the rapid growth of yeast. This causes an infection of the hair follicles and acne-like symptoms to appear. From pimple-like bumps to irritated skin, fungal acne is rather unpleasant and has a variety of causes.
Here are some common conditions or events that can upset the balance of bacteria and fungus on your skin:
Treatment of fungal acne is often delayed due to its similarities to bacterial acne. Often people would treat it with regular acne skincare treatments. However, this can irritate the surrounding skin and make the infection worse.
Some common fungal acne symptoms include:
While some of these symptoms can be mistaken for bacterial acne, it’s important to take note of the differences so as to avoid worsening the infection. In learning how to differentiate fungal acne from bacterial acne, you will be able to avoid worsening the infection and ultimately speed up the recovery process.
Here are some major differences between fungal and bacterial acne:
Fungal acne has shown to have a high incidence of recurrence once treated. However, there are plenty of ways to prevent fungal acne from occurring in the first place simply by keeping your skin clear and healthy.
Here are some steps you can take to prevent fungal acne:
Removing the conditions in which yeast thrive is the best way to prevent fungal acne from occurring. Yeast need hot and humid conditions to thrive – by wearing more breathable fabric, maintaining good personal hygiene and showering right away after exercising, these steps will help you avoid conditions that may increase your risk of a fungal acne.
In treating fungal acne, there are two main types of treatment:
Oral treatment is often the most effective option for treating fungal acne, especially when it comes to controlling the initial symptoms. Depending on the severity of the fungal acne, your doctor will prescribe the most appropriate medication based on your current condition. The most common oral antifungal medication is Sporanox, whereas Accutane is often considered for more difficult cases.
The treatment process for fungal acne can take several months depending on several factors such as the strength of medication, the persistence of the infection, and your body’s response to the medication. Once outbreaks and itching are under control, your doctor will help develop a plan to slowly wean off the antifungal medication.
Over-the-counter fungal medication are often helpful in maintaining and preventing future episodes of fungal acne. Topical treatments often come in the form of an anti-dandruff shampoo that is to be used every day of the week or as per your doctor’s prescription.
The most common treatments are Nizoral or Selsun. These brands are readily available in your local chemist and can be easily bought online. To apply the medication, it needs to be applied in the shower and left on for 5 – 10 minutes prior to rinsing off thoroughly.
Fungal acne is a common infection and is usually easy to treat as long as it’s correctly diagnosed.
While managing fungal acne can be vastly different from managing the typical acne that you’re used to, fungal acne can often be prevented with consistent personal care and hygiene to prevent yeast overgrowth.
To learn more about identifying, managing, and preventing different health conditions, book a First Aid course with us today.

May 1, 2025
Pterygium, also known as surfer's eye, is an ocular surface disease characterised by a growth of limbal and conjunctival tissue over the cornea. Fortunately, you can practice many eye health habits to help prevent the development of pterygium and other risks.
April 3, 2025
Tuberculosis is a severe bacterial infection that mainly affects the lungs and other parts of the body, including the nervous system. This contagious disease can quickly spread in crowded areas when an infected person coughs, talks, or sneezes.

February 13, 2025
Melioidosis is a bacterial infection caused by Burkholderia pseudomallei, a microorganism found in soil and water. This infection is often underdiagnosed due to symptoms mimicking many other illnesses. As such, awareness is critical for those living or working in affected regions.